Dementia is a neurodegenerative disease that can affect rational thinking and can lead to poor functioning with daily activities such as personal care, medication management and more.
When dementia is in its early stages, individuals may still be able to live independently with a few modifications or supports. However, as the disease progresses, there may be safety concerns or an inability to care for oneself.
This article will discuss some of the signs that someone with dementia requires 24 hour care and suggest some options that can be explored prior to receiving around the clock support.
Signs that dementia patients may be unable to live independently and care for themselves
Dementia can present itself in many ways, however some signs that someone may be unsafe to live independently and care for themselves include:
Confusion and wandering behaviors
Wandering behavior is a common sign of having advanced dementia, and can be dangerous because of the risk of getting lost or hurt.
For example, individuals may leave the home ill prepared for the elements and outdoor weather. There have been numerous cases of people with cognitive impairments going outside during the cold of winter without coats or warm clothing and freezing to death when they get lost and are unable to return home.
On top of this, searching for a lost member of the family can be particularly stressful for caregivers and police involvement can provoke emotional distress.
Another sign of mental impairment is difficulty with memory. For example, having poor orientation to facts that should be well known such as date of birth, home address and the current date can give clues that someone may have an impairment with their thinking.
This confusion and poor orientation can make it not only difficult to communicate with others, but also challenging to accomplish other important tasks such as banking, managing the finances and more.
Poor medication management and compliance
Another sign of trouble for those with dementia is issues with medication compliance. Not remembering to take medication as prescribed has a cascading effect that can contribute to further decline in rational thought from poor disease control.
For instance, periods of memory lapses can worsen or become more frequent resulting in forgetting to take medication or being resistant to treatment. In turn, this can make one’s mental state and rational thinking even worse and lead to further poor choices and decisions with everyday living and functioning.
Poor nutritional intake
To the surprise of many, dementia also affects the taste buds and can lead to changes in eating habits. For example, some individuals report that they do not experience flavor the same way as before and adopt new food preferences.
This can lead to snacking on more finger foods loaded with high fat, sugar and salt content. These snacks are usually considered unhealthy because they contain few nutrients needed to maintain muscle mass and optimal cognitive functioning.
Not bathing or dressing
An area where dementia patients tend to struggle is bathing and dressing. Cognitively impaired individuals may be resistant to engaging in personal care tasks or forgetful.
For example, those with dementia may get confused or disoriented resulting in shirts or pants being put on backwards or inside out.
It is also common for them to dress inappropriately for the temperature and weather ie. only wearing a shirt and shorts during a cold winter.
With bathing, some individuals may be resistant to maintaining their personal hygiene and may have body odor. It is not uncommon for dementia sufferers to reject a family member’s suggestion to have a shower or bath.
Struggling with basic mobility
Seniors are more likely to have difficulty with mobility due to frailty or other medical conditions. When this trouble is combined with dementia, walking can be particularly dangerous.
For instance, someone may need to utilize a cane or rollator walker for their safety. However, those with a cognitive impairment are more likely to forget to use these mobility devices or use them in an unsafe manner. This can place them at higher risk of falling, which can result in significant injury or death.
Options to explore prior to starting 24 hour care for dementia patients
Many caregivers wonder, when should a dementia patient go to a nursing home? For most people, the answer is when they have exhausted all other community support options and the person remains unsafe to live at home.
These are some common dementia supports and resources that may help avoid a nursing home admission:
Get increased help from family and support networks
When someone has lost the capacity to manage their day to day functioning and cannot fend for themselves, a good support network of friends and family can help these individuals age safely within their home.
A family unit that provides increased support can sometimes mean the difference between a nursing home admission and aging in place.
Examples of how a good support network can assist someone with dementia include:
- Navigate the healthcare system to arrange medical appointments, schedule diagnostic testing, facilitate home care support visits and discover other community resources
- Assist with bathing, dressing and other personal care activities
- Provide support with instrumental activities of daily living such as financial management, medication administration, housekeeping, home maintenance and repairs, and meal preparation
- Find and arrange alternate living arrangements if someone is no longer safe to live alone within their home
Use social assistance programs and home care services
Home care support either privately paid or through government social assistance programs are one way to help dementia patients and the cognitively impaired elderly cope with living at home.
Through government funding, the role of the healthcare aides is usually limited to essentials like bathing and dressing. When paying for service out of pocket, their scope of care can be expanded to other tasks such as meal preparation, medication administration, light housekeeping and more.
When accessing home care support through public funding, there may be an initial wait period before someone is evaluated for eligibility and services are arranged to visit. In contrast, privately paid care can usually commence a lot faster and with fewer restrictions on their purpose and role.
Family members rely on external caregivers because dementia patients are sometimes more receptive to instructions and guidance from non-relatives or professional caregivers. Other times, it is because the family members do not feel comfortable with seeing an individual naked to help them with personal care tasks such as bathing or dressing.
Explore living on a memory floor of a retirement home
When sufficient care and supervision cannot be provided within the person’s home, a dementia sufferer may need to move into a retirement home that has an enhanced service floor such as a memory unit.
On these memory units, nurses and non-medical health care aides are staffed around the clock to provide healthcare and personal care support as needed.
That said, this service is prohibitively expensive for most people. Many families, out of financial concern and worry about long term affordability, ultimately request to transfer to a nursing home where fees are somewhat subsidized by government bodies and social assistance.
Use assistive aids to improve safety at home
Safety equipment in the home are meant to help individuals struggling with bathing and dressing, be more safe, independent and less reliant on caregiver support.
Some common equipment found in a dementia patient’s home include:
- Transfer aids – grab bars, tub railings, tub transfer benches can be used to help someone with get into or out of the bathtub
- Bathing aids – sit on bath chairs, stools or bath benches to rest when showering and help with fatigue or balance issues
- Fall alert buttons – worn on the body, these buttons can be pushed to get help if one were to fall
Use mobility aids to make walking more safe
To help with walking, canes or rolling walkers can be used to improve stability and balance.
However, dementia patients frequently forget to use these devices and attempt to walk without support, often resulting in falls.
To help mitigate this, a bed or chair exit alarm sensor system can be used to alert nearby caregivers that someone is attempting to stand up. The caregiver can then remind the individual to use their mobility aid so they do not have a fall.
Alternatively, if the dementia is in its early stages and an individual can still comprehend the purpose of the alarm, it is possible that they would use this auditory cue as a reminder to use their walking cane or walker.
Consider dressing tags to achieve more independence
People with dementia and cognitive impairments frequently struggle with dressing due to being distracted easily or forgetting how to dress appropriately for the weather.
Some caregivers have found color coded clothing tags can be a helpful way of teaching dementia patients how to dress again and may help them achieve some level of independence.
For example, these tags can also be used as a guide to match weather appropriate clothing combinations, highlight which side is inside or out, and show which is the front and back of the clothing.
That said, using tags requires planning as caregivers must obtain and attach them to any clothing.
In some cases, this strategy may not be sufficient for a dementia patient to achieve dressing independence, and cues or supervision will continue to be required.
Caregivers can provide support by organizing what to wear for the day by laying clothing out. Also, they can provide guiding cues to ensure that clothing is put on correctly and gently remind dementia sufferers to focus on getting dressed.
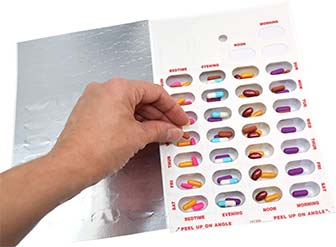
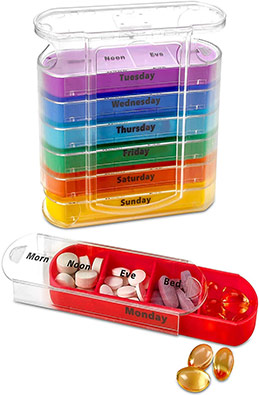
Use medication aids to improve compliance and memory
Individuals with cognitive impairments can easily forget to take their medication. These people may be able to achieve some level of independence with the use of medication aids.
Common medication aids for dementia patients include:
- Blister pack – med sheet typically organized by the pharmacy into different bubbles that contain all the medication someone needs to take at different times of the day
You can also make your own blister package by organizing do it yourself med sheets.
- Pill organizers – a pill container that is self organized on a weekly basis to keep track of medication administration
- Pill alarms – noise generating device that rings at preset times to remind someone to take their medication
- Automatic pill dispensers – device that releases medication at pre-programmed intervals to reduce medication errors
- Medication check in services – service that calls to remind someone to take their medication
Use herbs and spices to improve appetite
To improve the nutritional intake of someone with dementia, try introducing a variety of spices and herbs into foods.
Adding spices can make people more receptive to otherwise bland foods. This can be used to increase their intake of more nutritious foods that sometimes lack taste compared to unhealthy snack foods.
Examples of spices and herbs that can be used to improve a dementia patient’s appetite include:
- Chilli pepper
- Paprika
- Cayenne
- Turmeric
- Ginger
- Garlic
- Cloves
Tip: Always be aware of any food allergies and consult a physician or dietician prior to any dietary changes.